Breast cancer is a kind of cancer that develops from breast cells.
Every organ in the body is made up of various kinds of cells. Cells normally divide in an orderly way to produce more cells only when they are needed. Occasionally, cells become abnormal and divide without control. When this happens, they form a tumor, which can be benign or malignant.
Benign tumors are not cancerous and are not life threatening. Cells in the benign tumor do not invade other tissues and do not spread to other parts of the body. Malignant tumors are cancerous. They can invade and damage nearby tissues and organs. Cancer cells can enter the bloodstream or lymphatic system and spread to form secondary tumors in other parts of the body. The spread of cancer is called metastasis.
Breast cancer usually starts off in the inner lining of milk ducts or the lobules that supply them with milk. A malignant tumor can spread to other parts of the body. A breast cancer that started off in the lobules is known as lobular carcinoma, while one that developed from the ducts is called ductal carcinoma.
Breast cancer is the most common invasive cancer in females in India. It accounts for 30% of all female cancers and 22.9% of invasive cancers in women.
Breast cancer rates are much higher in developed nations compared to developing ones. There are several reasons for this, with possibly life-expectancy being one of the key factors breast cancer is more common in elderly women; women in the richest countries live much longer than those in the poorest nations. The different lifestyles and eating habits of females in rich and poor countries are also contributory factors.
What causes breast cancer?
There are many risk factors that increase the chance of developing breast cancer. Although we know some of these risk factors, we don’t know the cause of breast cancer or how these factors cause the development of a cancer cell.
We know that normal breast cells become cancerous because of mutations in the DNA, and although some of these are inherited, most DNA changes related to breast cells are acquired during one’s life.
What are breast cancer risk factors? How do you get breast cancer?
Some of the breast cancer risk factors can be modified (such as Oral contraceptive pills use) while others cannot be influenced (such as age). It is important to discuss these risks with a health-care provider anytime new therapies are started (for example, postmenopausalhormone therapy).
Several risk factors are inconclusive (such as deodorants), while in other areas, the risk is being even more clearly defined (such as alcohol use).
The following are risk factors for breast cancer:
- Age: The chances of breast cancer increase as one gets older.
- Family history: The risk of breast cancer is higher among women who have relatives with the disease. Having a close relative with the disease (sister, mother, daughter) increases a woman’s risk.
- Personal history: Having been diagnosed with breast cancer in one breast increases the risk of cancer in the other breast or the chance of an additional cancer in the original breast.
- Women diagnosed with certain benign breast conditions have an increased risk of breast cancer. These include atypical hyperplasia, a condition in which there is abnormal proliferation of breast cells but no cancer has developed.
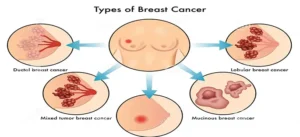
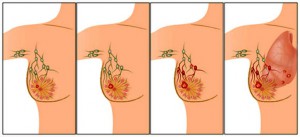
The single most important factor in assessing any breast cancer is determining whether it is noninvasive (in situ) or invasive. Noninvasive or in situ cancer confine themselves to the ducts or lobules and do not spread to the surrounding areas. There is one main type of noninvasive cancer: ductal carcinoma in situ (DCIS).
A diagnosis of DCIS is relatively good news. It means that abnormal cells are found only in the lining of the milk ducts of the breast, and that these abnormal cells have not spread outside the duct. DCIS has an extremely high cure rate. A diagnosis of LCIS means that the abnormal cells are found in the lining of the milk lobule. Although LCIS is not considered to be actual breast cancer at this noninvasive stage, it is a warning sign of increased risk of developing invasive cancer.
Invasive (or infiltrating) cancers are cancers that have started to break through normal breast tissue barriers and invade surrounding areas. Invasive cancers can spread to other parts of the body through the bloodstream and lymphatic system. Treatment for such cancers is generally more difficult but invasive cancers can often be cured in early stages.
Inflammatory breast cancer(IBC) is a rare but aggressive type of breast cancer. Its symptoms resemble an infection or allergic reaction, and are often the same symptoms found in some benign breast diseases, which makes diagnosis difficult. The breast may be red and painful and the skin may look like the peel of an orange. Inflammatory breast cancer grows and metastasizes rapidly. If symptoms similar to those listed above do not disappear when treated with antibiotics, a biopsy may be necessary to determine the diagnosis.
Paget’s disease is a rare cancer that begins in the milk ducts of the nipple. The symptoms include redness, oozing, crusting, itching, or burning of the nipple or a non healing wound. Any time there is a change in the appearance or condition of the breast, particularly if it persists beyond a few days, It should be checked and monitored by the doctor.
Age
The biggest single risk factor for breast cancer is age. The older a women gets, the greater is her likelihood of getting breast cancer. A women in her late 30s, for instance, has about a 1 in 257 chance of getting breast cancer. The risk increases exponentially after age 30,but even in women 80 years old, the risk of developing cancer is roughly 1 in 24.It means that, as women age, they need to be vigilant about watching for signs of changes in their breasts, because their risk has increased.
Personal History
Personal history includes women’s past medical history of breast cancer, ovarian cancer, uterine, or colon cancer. Women who have had any of these cancers previously stand a much greater chance of having a new cancer develop in their breast tissue. Breast cancer is also mildly related to the timing of normal physiological processes, such as menarche ( start of menstruation) and menopause (end of menstrual period).If a women’s menarche occurs prior to the age of 12,or if her menopause comes after the age of 55,or both, she stands slightly greater chance of developing breast cancer. Similarly, women who have had no pregnancies or whose first pregnancy occurred after age 30, are slightly at a greater risk than women who had pregnancy before this age. Breast feeding contributes to decreased cancer risk (the longer a women breast feeds, the lower her risk of breast cancer).
Family History
Many people believe that breast cancer is a disease that runs in families. Statistically speaking, this is not true. Over 80% of women who are diagnosed with cancer don’t have any family history of cancer. Nevertheless, women with a blood relative who has had breast cancer do have a greater risk, particularly if it’s a close relative (mother, sister, daughter).This is due to the fact that the cancer could have been caused by a mutation, or defective copy of gene, which might also have been inherited by her close relatives. Family history is significant if there are two or more close family members who have had breast and/or ovarian cancer, and if the breast cancer in the family members has been found before the age of 50.
Diet and physical Fitness
Women who are overweight or obese, particularly older women , also have a greater risk. Although there are no specific foods shown to increase one’s risk of breast cancer, numerous studies have shown that high levels of alcohol intake probably increase the risk of breast cancer. To decrease the risk for developing breast cancer, it is recommended that women consume a well-balanced diet rich in grains, fruits and vegetables, along with low consumption of fat and sugars and moderate consumption of meats, dairy products, eggs. Maintaining good physical fitness through exercise has been suggested as a potential way to lower cancer risk. Exercise reduces estrogen levels, fights obesity, lowers insulin levels, and boosts the immune system, all of which can aid in cancer prevention. There is some scientific evidence that women who have exercise regularly before menopause gain lifelong benefits against breast cancer, and a recent study showed that even moderate (four hours per week) exercise contributes to lower risk.
Oral contraceptive pills or hormone replacement therapy
Today, it is well known that the greater a women’s exposure to estrogen, the greater is her risk of developing breast cancer. A woman who starts menstruating early or goes through menopause late has a longer lifetime exposure to estrogen. A woman who hasn’t gone through childbirth or breast-feeding, both of which tend to suppress the menstrual cycle for extended periods of time, doesn’t get the risk lowering benefit of these events.
It is known that current or recent use of birth control pills (oral contraceptives) slightly increases the risk of breast cancer. Studies show that while women are taking birth control pills (and shortly after), they have a 20 to 30 percent higher risk of breast cancer than women who have never used the pill. Once women stop taking the pill, their risk begins to decrease and after about 10 years, returns to that of women who have never taken the pill.
Hormone replacement therapy (HRT) after menopause (Estrogen progesterone preparations) is linked to a higher risk of breast cancer. The longer the HRT is used, the higher the risk. The risk returns to that of a woman who never used HRT (the usual risk) within 3 years of stopping the hormones. Taking HRT is also linked to increased breast density (as seen on a mammogram). Increased breast density can make it harder to find breast cancer on a mammogram.
Myths
It is important to know the difference between what is a genuine risk factor and what is a myth. It is not possible to get breast cancer from contact with a person who has it. Nor it is possible to get cancer from a bruise, bump, or similar injury. Having large or small breasts neither increases nor decreases the risk of cancer. Claims that antiperspirants and underwired bras cause breast cancer by blocking the flow of sweat have not been substantiated by any scientific evidence.

8 Ways to Prevent Breast Cancer
1. Keep Weight in Check
It’s easy to tune out because it gets said so often, but maintaining a healthy weight is an important goal for everyone. Being overweight can increase the risk of many different cancers, including breast cancer, especially after menopause.
2. Be Physically Active
Exercise is as close to a silver bullet for good health as there is, and women who are physically active for at least 30 minutes a day have a lower risk of breast cancer. Regular exercise is also one of the best ways to help keep weight in check.
3. Eat Your Fruits & Vegetables – and Avoid Too Much Alcohol
A healthy diet can help lower the risk of breast cancer. Try to eat a lot of fruits and vegetables and keep alcohol at moderate levels or lower (a drink a day or under). While moderate drinking can be good for the heart in older adults, even low levels of intake can increase the risk of breast cancer. If you don’t drink, don’t feel you need to start. If you drink moderately, there’s likely no reason to stop. But, if you drink more, you should cut down or quit.
4. Don’t Smoke
Smokers and non-smokers alike know how unhealthy smoking is. On top of lowering quality of life and increasing the risk of heart disease, stroke, and at least 15 cancers – it also causes smelly breath, bad teeth, and wrinkles. Now that’s motivation to stay smoke-free or work to get smoke-free.
5. Breastfeed, If Possible
Breastfeeding for a total of one year or more lowers the risk of breast cancer. It also has great health benefits for the child.
6. Avoid Birth Control Pills, Particularly After Age 35 or If You Smoke
Birth control pills have both risks and benefits. The younger a woman is, the lower the risks are. While women are taking birth control pills, they have a slightly increased risk of breast cancer. This risk goes away quickly, though, after stopping the pill. The risk of stroke and heart attack is also increased while on the pill – particularly if a woman smokes. If you’re very concerned about breast cancer, avoiding birth control pills is one option to lower risk.
7. Avoid Post-Menopausal Hormones
Post-menopausal hormones shouldn’t be taken long term to prevent chronic diseases, like osteoporosis and heart disease. Studies show they have a mixed effect on health, increasing the risk of some diseases and lowering the risk of others, and both estrogenonly hormones and estrogen-plus-progestin hormones increase the risk of breast cancer. If women do take post-menopausal hormones, it should be for the shortest time possible. The best person to talk to about the risks and benefits of post-menopausal hormones is your doctor.
8. Tamoxifen and Raloxifene for Women at High Risk
Although not commonly thought of as a “healthy behavior,” taking the prescription drugs tamoxifen and raloxifene can significantly lower the risk of breast cancer in woman at high risk of the disease. Approved by the FDA for breast cancer prevention, these powerful drugs can have side effects, so they aren’t right for everyone. If you think you’r eat high risk, talk to your doctor to see if tamoxifen or raloxifene may be right for you.

The first symptom of breast cancer most women notice is a lump or an area of thickened tissue in their breast.
Most breast lumps (90%) aren’t cancerous, but it’s always best to have them checked by your doctor.
Breast awareness
It’s important to be breast aware so you can pick up any changes as soon as possible.
Get to know what is normal for you – for instance, your breasts may look or feel different at different times of your life. This will make it much easier to spot potential problems.
Symptoms of breast cancer
Other symptoms which may be noticed in the affected breast include:
- Changes in the size or shape of a breast.
- Dimpling or thickening of some of the skin on a part of a breast.
- The nipple turning in (becoming inverted).
- Rarely, a discharge occurring from a nipple (which may be bloodstained).
- A rare type of breast cancer, causing a rash around the nipple, which can look similar to a small patch of eczema.
- Rarely, pain in a breast. Note: pain is not a usual early symptom. Many women develop painful breasts (mastalgia) and this is not usually caused by cancer.
How is breast cancer diagnosed?
Initial assessment
If you develop a lump or symptoms which may be breast cancer, a doctor will usually examine your breasts and armpits to look for any lumps or other changes. You will normally be referred to a specialist. Sometimes a biopsy of an obvious lump (see below) is arranged, but other tests may be done first such as:
- Mammogram. This is a special X-ray of the breast tissue.
- Ultrasound scan of the breast.
- MRI scan of the breast. This is more commonly performed on younger women, who may have denser breast tissue.
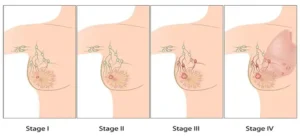
What is Cancer Staging?
Cancer staging is the process of determining how much cancer is in the body and where it is located. Staging describes the severity of an individual’s cancer based on the magnitude of the original (primary) tumor as well as on the extent cancer has spread in the body. Understanding the stage of the cancer helps doctors to develop a prognosis and design a treatment plan for individual patients.
Staging provides a common language for doctors to effectively communicate about a patient’s cancer and collaborate on the best courses of treatment.Understanding the cancer’s stage is also critical to identifying clinical trials that may be appropriate for particular patients.
What are the Different Types of Staging?
There are four different types of staging:
-
Clinical Staging determines how much cancer there is based on the physical examination, imaging tests, and biopsies of affected areas.
-
Pathologic Staging can only be determined from individual patients who have had surgery to remove a tumor or explore the extent of the cancer. Pathologic staging combines the results of both the clinical staging (physical exam, imaging test) with surgical results.
-
Post-Therapy or Post-Neoadjuvant Therapy Staging determines how much cancer remains after a patient is first treated with systemic (chemotherapy or hormone therapy) and/or radiation therapy prior to their surgery or where no surgery is performed. This can be assessed by clinical staging guidelines and/or pathologic staging guidelines.
-
Restaging is used to determine the extent of the disease if a cancer comes back after treatment. Restaging helps determine the and the best treatment options for cancer that has returned.
What are the Common Elements of Staging Systems?
Staging is based on commonly understood knowledge about the way cancer develops and spreads.
In most cases, the stage is based on four main factors:
-
Location of the primary (original) tumor
-
Tumor size and extent of tumors
-
Lymph node involvement (whether or not the cancer has spread to the nearby lymph nodes)
-
Presence or absence of distant metastasis (whether or not the cancer has spread to distant areas of the body)

Which treatments are used for breast cancer?
There are several ways to treat breast cancer, depending on its type and stage.
Local treatments: Some treatments are called local therapies, meaning they treat the tumor without affecting the rest of the body. Types of local therapy used for breast cancer include:
- Surgery
- Radiation therapy
These treatments are more likely to be useful for earlier stage (less advanced) cancers, although they might also be used in some other situations.
Systemic treatments: Breast cancer can also be treated using drugs, which can be given by mouth or directly into the bloodstream. These are called systemic therapies because they can reach cancer cells anywhere in the body. Depending on the type of breast cancer, several different types of drugs might be used, including:
- Chemotherapy
- Hormone therapy
- Targeted therapy
Many women will get more than one type of treatment for their cancer.
How breast cancer is typically treated?
Most women with breast cancer will have some type of surgery to remove the tumor. Depending on the type of breast cancer and how advanced it is, you may need other types of treatment as well, either before or after surgery, or sometimes both. Surgery is less likely to be a main part of the treatment for more advanced breast cancers.
Typical treatment plans are based on the type of breast cancer, its stage, and any special situations:
- Invasive breast cancer (stages I-IV)
- Ductal carcinoma in situ (DCIS)
- Inflammatory breast cancer
- Breast cancer during pregnancy
Your treatment plan will depend on other factors as well, including your overall health and personal preferences.
Who treats breast cancer?
Doctors on your cancer treatment team might include:
- A breast surgeon: a doctor who uses surgery to treat breast cancer
- A radiation oncologist: a doctor who uses radiation to treat cancer
- A medical oncologist: a doctor who uses chemotherapy and other medicines to treat cancer
Many other specialists might be part of your treatment team as well, including physician assistants, nurse practitioners, nurses, psychologists, social workers, nutritionists, and other health professionals.

Mastectomy and breast conservation surgery
The surgical procedures most commonly referred to by the term mastectomy are total (simple) mastectomy, in which the surgeon removes the whole breast but does not remove lymph nodes, and modified radical mastectomy. in which the surgeon removes the breast, all lymph nodes under the arm, and the lining over the chest muscles. Simple mastectomies are used primarily for noninvasive cancers while modified radical mastectomies are used when there is a possibility of cancer having spread to the lymph nodes.
In a breast conservation surgery, the tumour along with a surrounding margin of normal breast tissue is removed. However radiation therapy is essential after breast conservation surgery.
Treatment of lymph nodes under arm
If there is a suspicion of lymph nodes being involved with cancer, then all the lymph nodes are removed. This is called axillary lymph node dissection. This causes some post operative complications like- swelling in the arm (known as lymphoedema), seroma (persistent fluid collection in the armpit), tingling numbness and pain in the upper inner arm and restriction of shoulder movement. To avoid these complications, a procedure called sentinel node biopsy is used, in which a dye is injected around the tumour before surgery and the first or primary nodes which are draining that area are identified and removed. They are then sent to the pathologist. If the pathologist reports the nodes as having no tumour cells, then nothing more is done, If the pathologist reports the nodes as positive for tumour cells, then complete lymph node dissection is done. In this way, unnecessary axillary dissection can be avoided for patients with negative lymph nodes in the armpit.
Breast reconstruction
If complete removal of the breast (mastectomy) is required, then reconstruction of the breast can be done. This can be done as an immediate procedure at the time of mastectomy or delayed procedure which is after completion of all treatment. Reconstruction provides emotional and psychological benefit to the patient apart from the obvious cosmetic improvement. There are a number of options for reconstruction- autologous (in which the other body tissues are used to artificially reconstruct the breast) and implant based (in which silicon implants are used to reconstruct the breast). A number of factors affect the choice of reconstruction like- the volume of breast to be reconstructed, skin elasticity, tumour size and location, need for radiation, body habitus etc.

What Is Radiation Therapy And How Does It Work?
Radiotherapy is the use of high energy X- rays to damage cancer cells and stop them from growing. The radiation is very carefully targeted to affect a limited number of cells- any remaining cancerous cells and a very small portion of surrounding normal cells in order to minimize damage to normal tissues. The goal is to kill the diseased tissue and spare the normal ones. Radiation therapy is most commonly given after completion of chemotherapy. Radiation can be given as external beam ( in which X rays come from radiation material outside the body) or brachytherapy (in which radioactive material is directly placed in the breast in thin tubes). External radiation therapy is more commonly used and is usually given for a period of 5-6 weeks for 5 days per week. At the end of the therapy an additional boost is often given that is focused on the primary site of the tumour.
"Health is the most important thing you have in life!"
Contact us now to schedule an appointment.